The importance of radiation safety in interventional surgery
X-ray is used for guidance in a wide range of surgical procedures, for treatments mostly related to dysfunctions in various organs such as heart, liver, kidneys and lungs. Such procedures can be lengthy, and the surgical team is always present in the operating room, which means they get accumulated doses over time.
Due to scattered radiation, it is hard to know where it is optimal to stand to get as low dose as possible and still be able to work efficiently. If a patient is large, he/she will absorb more radiation, which will spread to the staff.
The problem with radiation is that you can´t see it and you can´t feel it, but it´s there, and it effects us. What is worse, we don´t know what threshold would give a problem such as cataract or cancer, so we must assume there is no safe level of radiation!
Methods have improved, and medical equipment is more effective which have contributed to drastically reduced doses. ALARA (As Low As Reasonably Achievable) principles guide us to use various shielding, decrease exposure time and distance to source. We strive to decrease the field of operation by adjusting machine parameters e.g decrease frame rate, and adjust the angle of the X-ray tube. Still there is more to do.
How real-time dosimetry can be used for continuous improvements
With real-time dosimetry each staff individual can see their radiation dose in real-time, enabling them to see and take action to reduce their exposure as it happens and not just after, when readings from legal dosimeters are reported back.
If the team is getting a high dose, they can check if for instance the under-table-protection or shielding hanging from the ceiling are inadequate, if there is a gap between radiation protection pieces or something else that requires their attention. Real-time dosimetry is a powerful tool that helps the team to improve and take control of their own situation.

How it works
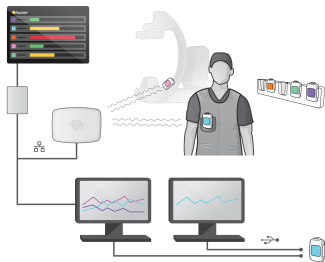
Each staff member wears a real-time dosimeter which measures and records radiation every second. Dose data is transferred and displayed as color-coded bar graphs for up to eight individuals at the same time. This visual feedback can alert them to take action to avoid unnecessary radiation.
The RaySafe i3 system is developed by the inventor of the visual real-time dosimetry technology, and it comes in two main configurations:
• RaySafe i3 with Stand-alone Display (Real-time view on the RaySafe Real-time Display)
• RaySafe i3 with On-screen Display (Real-time view on the X-ray System´s main monitor)

Watch how-to-video:
Introduction to RaySafe i3
Watch webinar:
Instantly Control Your Radiation Dose
Scatter Matters
RaySafe i3 Demo Day
Read more in:
Real-time Dosimetry Product Catalog
RaySafe i3 Product Brochure
RaySafe Real-time Dosimetry Brochure (incl On-Screen Display)
Suitable products for measuring real-time dose
Real-time dosimetry and best practices for radiation safety
In Chapter 4.3 of “2023 Clinical Practice Guidelines on Radiation Safety”, European Society for Vascular Surgery (ESVS) recommends real-time dosimetry to be considered by all personnel in the endovascular operating room. In addition to other personal dosimetry. Real-time dosimeters are also called APD:s (Active Personal Dosimeters) which are defined to provide immediate and continual measurement of radiation exposure that can be visible to the staff member during a procedure.
Links to Scientific Reports
Effects of Real-Time Dosimetry on Staff Radiation Exposure in the Cardiac Catheterization Laboratory

The history of visual real-time dosimetry
During the European Congress of Radiology in Vienna 2012, Unfors RaySafe launched the RaySafe i2 real-time dosimetry system. It was now possible for medical staff to get real-time insights about their individual radiation exposure during imaging procedures. Getting instant information on current X-ray exposure levels provides enhanced knowledge and prerequisites to minimize unnecessary exposure. Time-stamped dose data collected by RaySafe i2 allowed for streamlined work processes and improved workplace efficiency and safety. Studies indicated a reduction in dose to personnel of up to 40% when using Unfors RaySafe’s real-time dosimetry technology. In March 2017, the current RaySafe i3 real-time dosimetry system was introduced to the market. The RaySafe i3 is designed to improve wearability, with a prolonged life cycle and increased measurement accuracy. The device can be used in low-dose procedures and in hybrid operating room (OR) environments.

